The #gyncsm community started in 2013 after both Christina and I took part in a #bcsm chat on dealing with recurrence.
After eleven years, we
have made the difficult decision to cease hosting the #gyncsm chat. Our
last chat will be on Wednesday, December 11, 2024 at 8pmET with guest and long-time supporter, Cervivor (@IamCervivor).
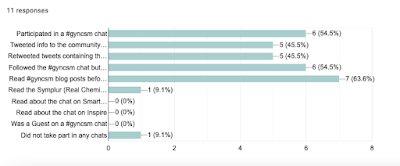
Our decision is based on a
number of reasons including the change in the X/Twitter platform since we held our first chat in 2013, the reduced number of chat participants - especially patients and survivors over the past year (see survey summary) - and the migration of health care providers, organizations, and cancer advocates like the Advocates for Collaborative Education (ACE) to alternate platforms. Dee will continue to use the
#gyncsm hashtag on X. We hope that others will continue to use the #gyncsm hashtag to share research studies, research results, highlights from oncology meetings, and to connect with others. We will leave the @gyncsm profile page open on X but will not be updating it.
We want to take this time to thank our current and former healthcare moderators:
Dr. Shannon Westin (2015-2024)
Dr. Nita Lee (2024)
Dr. Ann Becker-Schutte (2013-2024)
Dr. Sarah M. Temkin (2018-2022)
Dr. Rick Boulay (2013-2020)
Dr. Merry J. Markham (2013-2018)
Dr. Don S. Dizon (2013-2015)
We are also grateful for for the strong support throughout the years from Dr. Matthew Katz, the Society of Gynecologic Oncology/Foundation for Women's Cancers, Smart Patients, and Cervivor.
We thank the researchers including Teresa Hagan, Dr. Laura Harvelisky, and Dr. Lauren Hand who joined with us to learn about the needs of women with ovarian cancer, the needs of caregivers, and PARP decision making for patients. You can find those published articles here on our blog at http://gyncsm.blogspot.com/p/publications.html
We can’t forget to thank the social media gurus who we joined with to study cancer hashtag communities including Dr. Matthew Katz, Patricia Andersen, Audun Utengen, and Dr. Mike Thompson. Thank you! You can also find those articles here on our blog at http://gyncsm.blogspot.com/p/publications.html
We appreciate the numerous guests through the years who have shared their expertise on gynecologic cancers, as well as emotional and physical support topics. Thank you to the countless gynecologic oncologists, medical oncologists, radiation oncologists, nurses, social workers, therapists, and other health care providers who shared their knowledge and helped our community. We also appreciate the information you shared from ASCO, SGO, and other annual meetings. A shout-out to all the researchers who have shared their published journal articles, answered questions, and listened to the patients/survivors in our community
And finally we want to thank the the numerous #gyncsm patients, previvors, survivors, and caregivers that have joined our chats the past 11 years. You are why we started this community. We hope we have provided a safe place to share, ask questions, and learn.
We'll see you on December 11th for our final chat. Below are the questions that will guide our discussion:
T1: Before we dive into treatment advancements, let's cover some important #cervicalcancer basics:
What are the current cervical cancer screening guidelines?
What are the recommendations for receiving the HPV vaccine?
T2: What are some of the recent advances in the treatment of #cervicalcancer in the areas of immunotherapy, targeted therapy, radiation therapy, etc?
T3: Have there been advancements in the treatment of recurrent #cervicalcancer?
T4: How can #cervicalcancer patients stay up-to-date on the latest treatments and what is the best way to find a clinical trial?
T5: What are the WHO initiatives regarding #cervicalcancer and global efforts to reduce disparities and eradicate cervical cancer? What can we do locally to reduce disparities?
T6: Please share #cervicalcancer resources that you have found helpful.
Dee and Christina
Co-founders and co-moderators


.png)